The Respiratory and Circulatory Systems
They work together to provide gas and nutrients to the body and to eliminate waste.
The primary purpose is Gas Exchange.
Because the entire body relies on these two systems for virtually uninterrupted gas exchange, responses in them induced by the underwater environment can affect every cell in the body.
Circulatory System:
Oxidative metabolism is the process which cells use oxygen to convert chemical energy into usable energy required to sustain life. All the living cells in the body do this. Tissues can die rapidly without an uninterrupted oxygen supply.
And so, the circulatory system transports oxygen, fuels and materials from the respiratory and digestive system to your body tissues.
It carries waste, CO2 and other wastes, from your tissues for elimination.
The transport of gases to and from the respiratory system is the most important and relevant to diving.
Blood is an important part of this system accomplishing many functions: supplying oxygen and carrying away carbon dioxide are especially relevant to the circulatory system. Although it fulfills other functions such providing nutrients, carrying away waste, mobilizing the immune system etc.
Plasma is the actual liquid that carries the nutrients and also dissolved gasses including some of the waste carbon dioxide produced by the cells away from the tissues in the form of bicarbonate. By transporting carbon dioxide in the form of bicarbonate, the circulatory system carries more than it could by direct solution into the plasma alone. It also carries dissolved nitrogen as it fluctuates with the partial pressure of breathed nitrogen (this information is also from physics and the RDP sections).
However it carries little dissolved oxygen. Red blood cells carry the majority of the oxygen necessary for the body via hemoglobin. If the blood did not contain hemoglobin, the blood would have to circulate the plasma 15-20 times faster to meet oxygen demands, and this is assuming you are completely at rest.
Due to a high oxygen partial pressure (PO2) in the lungs, oxygen dissolves into red blood cells to bond with the hemoglobin. Along the way to the body’s tissues, metabolism consumes the oxygen resulting in a lower PO2. With much of this oxygen released, the hemoglobin can now bind reversibly with carbon dioxide and carry it to the lungs for elimination along with the carbon dioxide transported within the plasma.
Respiratory System:
Broadly speaking, all gases entering or leaving your body do so in your lungs – part of the respiratory system. The basic sequence involved in the physiology of breathing is as follows:
Primarily, it carbon dioxide which controls breathing NOT oxygen. The urge to breathe comes when the body detects increases carbon dioxide levels and/or a decrease of oxygen in the blood and tissues (but as mentioned, CO2 is usually the trigger).
The reflex respiratory centres in the brain PRIMARILY control the breathing by detecting CO2 levels higher than average. However, peripheral chemo-receptors in other areas monitor oxygen levels and may signal your respiratory centres when a decline in PO2 is detected.
If oxygen levels are normal but there is an overabundance of CO2 in the system, the reflex respiratory centre stimulates breathing. This is an important concept regarding breath-hold diving (discussed later).
Inhaling- the diaphragm flexes downwards thus increasing the chest’s internal volume. Internal pressure decreases and causes air to flow inward.
Exhalation – the diaphragm relaxes allowing the elasticity of the lungs to contract, forcing the air from the lungs as internal volume decreases and internal pressure increases.
Circulatory and Respiratory Systems Organs, Structure and Functions
The circulatory system (or cardiovascular system) consists of the heart, veins, arteries, and capillaries and circulates blood through the body as a closed circuit system.
Heart:
The heart is divided into two sides. Each side is divided again into two chambers, the atrium (upper chamber) and ventricle (lower chamber).
Each chamber has a sort of one-way valve at its exit that prevents blood from flowing backwards. When each chamber contracts, the valve at its exit opens. When it is finished contracting, the valve closes so that blood does not flow backwards.
Blood vessels (veins):
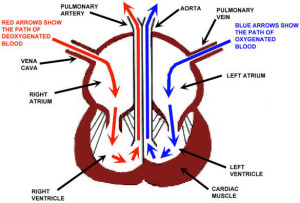 The blood vessels carry blood to the heart from the rest of the body. This blood carries carbon dioxide and cellular waste products. The blood goes into the right atrium and then to the right ventricle, where it is then pumped to the lungs to dispose of wastes and receive a fresh oxygen supply. From the lungs, the blood returns to the heart. It returns to the left atrium and then to the left ventricle. The blood is then pumped out of the heart by the left ventricle into the aorta. The left ventricle is the chamber of the heart that is responsible for pumping blood to all parts of the body. The aorta sends this blood to small arteries, which carry the oxygen-rich blood to the rest of the body.
The blood vessels carry blood to the heart from the rest of the body. This blood carries carbon dioxide and cellular waste products. The blood goes into the right atrium and then to the right ventricle, where it is then pumped to the lungs to dispose of wastes and receive a fresh oxygen supply. From the lungs, the blood returns to the heart. It returns to the left atrium and then to the left ventricle. The blood is then pumped out of the heart by the left ventricle into the aorta. The left ventricle is the chamber of the heart that is responsible for pumping blood to all parts of the body. The aorta sends this blood to small arteries, which carry the oxygen-rich blood to the rest of the body.
To summarize, the veins carry deoxygenated blood into the right side of your heart, and the arteries carry oxygenated blood away from the left side of the heart.
Respiratory System:
Ribs, intercostal muscles (between the ribs), diaphragm, lungs, mouth, nose, and a series of pipes connecting the mouth and lungs
On inhalation, air is passed from nose and mouth into the oral-nasal passages, the air then travels past the epiglottis (a valve between the trachea and oesophagus which leads into the stomach to prevent you from inhaling food or liquids) in the throat into the trachea (windpipe). Air travels down the trachea which divides into the right and left bronchi which enter the right and left lungs.
Within the lungs the bronchi continuously branch into smaller passages called bronchioles. Alveoli are located at the end of the smallest branches of the bronchi, which are air sacs surrounded by pulmonary capillaries. The walls/membranes of the capillaries are so thin that they are permeable, allowing gases to move freely between the alveoli and the bloodstream. This is where gas exchange takes place (the alveoli) into your blood (where the blood releases CO2 and picks up oxygen).
Remember that gas exchange between the respiratory system and the circulatory system occurs in the alveoli, but gas exchange between the tissues and the blood occurs in the capillaries.
Dead Air Space:
Dead air space is the portion of the tidal volume that plays no direct part in gas exchange.
Without equipment it consists of your sinuses, trachea and bronchi.
With equipment, the additional volume includes your snorkel, regulator or other breathing equipment.
When you inhale, the first gas drawn into your alveoli is the gas left in your breathing passages from your previous expiration. This gas is higher in CO2 than the fresh gas that you are breathing. Adding a snorkel or regulator increases the amount of dead air you inhale, this means that dead air becomes a larger portion of each breath thus raising the CO2 in the alveoli correspondingly.
Breathe deeply to maximise your tidal volume to avoid building up too high a level of carbon dioxide.
Breath-Hold Diving and Extending Breath-Hold Time
Apnea is the cessation of breathing. While breath-hold diving, the body responds to apnea.
During apnea, your circulatory system taps oxygen stored in your lungs, muscles and blood to supply tissue oxygen needs. Because you can’t vent the CO2, it builds up in your circulatory system, lungs, muscles and other organs, and thus raising CO2 causes the reflex respiratory centre to reflex in your diaphragm which you feel/interpret as the urge to breathe.
Relax and minimize effort, practise, also by intentionally hyperventilation with 3 or 4 deep rapid breathes prior to holding your breathe. This reduces the CO2 level to below normal delaying the urge to breathe.
Tachycardia is the speeding up of the heart rate. Bradycardia is the slowing of the heart rate.
When you first take a deep breathe, tachycardia occurs followed by bradycardia.
The bradycardia response to apnea has sometimes been called the mammalian diving reflex/mammalian reflex. This reflex is associated with cold water on the face. It can be said that the mammalian reflex is bradycardia response to apnea, or that the body responds to apnea in cool water with bradycardia.
Carotid-Sinus Reflex
As the brain cannot survive more than a few minutes without oxygen, the carotid-sinus receptors (located in neck which take blood up to brain), continuously monitor the blood pressure located in the carotid-sinus arteries.
The receptors send impulses to the cardio inhibitory centre in your brain which regulates the heart.
If the carotid-sinus receptors detect high blood pressure, they stimulate the cardio inhibitory centre which slows the heart rate. Similarly, if the receptors detect low blood pressure, they stop stimulating the cardio inhibitory centre which in turn stops sending signals to the heart thus increasing your heart rate.
Because of this process, if you wear a tight hood/dry suit (anything that constricts your neck), the carotid-sinus receptor may perceive this as high blood pressure and stimulate the cardio inhibitory to slow the heart. If this process continues (that is the heart rate slowing but the carotid-sinus receptors continue to perceive the pressure on the neck from the hood as high blood pressure), you may lose consciousness due to a reduced blood supply to your brain.
Hypercapnia
Hypercapnia is too much CO2 in the respiratory and circulatory systems. It can be the result of several things already discussed including dead-air space and holding your breath.
This can result in headache, confusion, accelerating breathing and eventual unconsciousness.
In scuba diving, the most common causes are high exertion, or failing to breathe slowly and deeply!!!
A combination of a high portion of dead-air and high levels of CO2 production, can result in CO2 being generated faster than the respiratory system can eliminate it. Once again, as mentioned earlier, the reflex respiratory centre stimulates you breathe faster. Due to greater density of gas at depth, the diaphragm and other respiratory muscles must work even harder. Again this produces more CO2 which stimulates even faster breathing. The circulatory and respiratory systems need to catch up with the body’s gas exchange rate; this is only accomplished if the diver stops all activity and rests.
Avoid hypercapnia by breathing slowly and deeply, avoiding overexertion underwater, skip breathing and contaminated air.
Hypocapnia and Shallow Water Black-Out
Hypocapnia is insufficient CO2. As you reflex respiratory centre regulates your breathing based primarily on CO2 levels, hypocapnia can also cause physiological problems.
Hypocapnia generally occurs following excessive voluntary hyperventilation (such as hyperventilating too much before a breathe-hold dive) or unintentional hyperventilation due to stress or fright.
Hypocapnia during breath-hold diving can lead directly to shallow-water blackout without the warning of symptoms e.g. light headedness, eventual fainting
Shallow-water blackout can occur if a diver hyperventilates too much at the surface, causing hypocapnia, – carbon dioxide levels drop thus dangerously reducing the urge to breathe. During the dive however, CO2 doesn’t return to a level that stimulates breathing before the tissues consume all the available oxygen. The diver stays underwater longer than normal and the body uses too much oxygen, but stays conscious due to the higher oxygen partial pressure. Upon ascending, the partial pressure drops significantly below the level that allows hemoglobin to bind with oxygen. This causes hypoxia (insufficient oxygen) and the diver blacks out without warning.
The most severe, tissue damaging hypoxia is anoxia– no oxygen at all.
Carbon monoxide
Breathing carbon monoxide under pressure while diving is more dangerous. Symptoms are not noticeable at depth because tissues may get adequate oxygen despite carbon monoxide binding with hemoglobin and so delays the onset of symptoms. Hypoxia may result (lack of oxygen supply to the tissues) and the diver blacks out without warning.
Carbon monoxide bonds with the haemoglobin over 200 times more readily than oxygen is able to, though does not unbound so easily. It can take the circulatory system 8-12 hours to eliminate it.
Victim’s lips and nail beds may turn bright red, although this is rare. This is because haemoglobin bonded with oxygen appears very red, and when the contaminated blood flows through the capillaries that are close to the skin, the lips and nail beds become redder. Due to colour absorption underwater, this may not always be apparent.
Smoking also raises carbon monoxide levels in the blood three to twelve times.
Symptoms of mild cases subside after several hours of fresh air. In severe cases, give the diver oxygen and contact emergency medical care.
Oxygen Toxicity
There are two types of oxygen toxicity: Pulmonary oxygen toxicity and central nervous system oxygen toxicity.
Pulmonary oxygen toxicity results from a lengthy exposure to PO2 greater than 0.5bar. It is a form of Oxygen poisoning that directly affects the lungs. It isn’t a significant concern (except in extreme cases where early symptoms have been ignored) even when it does occur. To avoid, don’t stay at PO2 of 0.5-1bar for long periods of time, and by following table guidelines and limits.
Lung irritation is the most immediate and most noticeable symptom, and may begin as a mild throat irritation followed by a cough. Severe cases may cause continuous burning in the chest and a continuous cough.
It is mostly a concern for tec divers not no stop recreational diving.
Central nervous system oxygen toxicity: involves nervous system reactions to oxygen exposure and tends to be unpredictable. It is the more serious toxicity and can cause a diver to drown. Only occurs if breathing PO2 above 1.4bar.
Remember the acronym VENTID when listing the symptoms:
V- visual disturbances (tunnel vision, blurring)
E- ear disturbances (ringing, music)
N- nausea,
T- twitching (especially in the face)
I- irritability
D- dizziness (vertigo)
The most serious symptom is a convulsion or hyperoxic seizure. Powerful and strong repeated contractions may cause unconsciousness. The concern with this underwater is that a diver may lose the regulator mouthpiece.
Physiological Mechanisms by which the Body Absorbs and Releases Nitrogen
Gas always goes from a higher pressure to a lower pressure. And so while diving, nitrogen dissolves into and out of the body tissues until that pressure of nitrogen dissolved in the tissues is the same as the surrounding pressure.
Different parts of the body absorb and release nitrogen at different rate (more about this concept in Decompression theory and RDP). However, most dives are too short for tissues to reach saturation.
Whilst ascending, the pressure of nitrogen that is dissolved in the body is higher than the pressure of nitrogen in breathing air, and so the nitrogen dissolves out of the body tissues into the breathing air and is exhaled. If the ascent is slow, then the pressure difference between the nitrogen dissolved in the body and the surrounding pressure (known as pressure gradient) is kept within the acceptable limits. The nitrogen in the body dissolves harmlessly out of the body and into the breathing air.
However, if the ascent is too fast, the difference in pressure of nitrogen dissolved in the body and the surrounding pressure (pressure gradient) is too great. Nitrogen comes out of solution faster than it can be eliminated from the body and forms bubbles (also covered in theory of physics) and may result in decompression sickness, DCS.
Silent bubbles
Some excess nitrogen dissolves to form tiny bubbles. These are so small they do not cause DCS. These bubbles travel through the venous system to the lungs, where the pulmonary capillaries trap them. The gas in these bubbles then diffuses harmlessly into your alveoli. (Except in rare cases where they accumulate faster than they diffuse as there as so many of them)
These bubbles are known as silent bubbles because they don’t produce DCS.
Decompression Sickness
There are two types of decompression sickness/ DCS:
Type I: ‘Pain only’, symptoms are not immediately life threatening
Type II: Symptoms that may be immediately life threatening involving the central nervous system
It is caused by bubbles of nitrogen forming in the tissues and bloodstream that block the flow of oxygen to the tissues.
Bubbles exist to some degree in the body after all dives. If the bubbles are to few and small (silent bubbles) they have no effect. However, if there are enough bubbles, their volume can be large enough to cause decompression sickness.
DCS may be delayed after a dive, and can take as long as 36 hours to manifest, although about half of DCS cases appear within an hour of the dive.
It can result from too rapid an ascent (physics theory).
Type I:
Pain only DCS that presents signs and symptoms that are not immediately life threatening or likely to cause long-term disabilities.
Type I may be broken down again into two categories:
1. Cutaneous decompression sickness results from bubbles coming out of solution in skin capillaries (also called the skin bends). Symptoms include a red rash in patches, usually on the shoulders and upper chest. Cutanaous DCS is not considered dangerous in itself, but may be an indication of further decompression problems and the possibility of more serious symptoms. If there are no other symptoms, it may be treated with oxygen breathing only and not require recompression.
2. Joint and limb pain decompression Sickness occurs in approximately 75% of DCS cases. Pain symptoms may be located in more than one place on the same limb e.g. the shoulder and elbow. In the short term it may be considered serious as it may progress to more severe form of DCS.
Type II:
This type of DCS has symptoms that may be immediately life threatening or debilitating, in particular to the central nervous system.
It may be broken down into three categories:
1. Neurological decompression sickness can produce some of the most serious cases. The nervous system reaches all parts of the body, and so movement, touch, life-support functions such as breathing and heartbeat can be affected. Signs and symptoms therefore include peripheral tingling and numbness, unconsciousness, respiratory arrest and paralysis. It usually affects the spinal cord thus causing numbness and paralysis in the lower extremities that move upwards. Without treatment, it can cause paralysis from the neck down.
2. Pulmonary decompression sickness manifesting itself in lung capillaries signals the onset of life-threatening symptoms. Usually (as mentioned earlier), when silent bubbles reach the pulmonary capillaries they usually diffuse into alveoli harmlessly. However, in rare cases or there is a large presence of silent bubbles, the gas accumulation can overwhelm the pulmonary capillaries to the point that bubbles travel through them into the arterial side of circulation. This can be the result of failure to follow dive tables or computers. A large presence of these bubbles can also block and back up blood flow to the lungs. Due to the reduction in oxygen flow to the tissues, symptoms include breathing pain commonly followed with a short, irritated cough. Also, a feeling of being air-starved may occur, and these symptoms tend to progress quickly and may lead to shock.
3. Cerebral decompression sickness results from bubbles passing through the pulmonary capillaries and travelling to the brain via the carotid arteries. Symptoms include blurred vision, headache, confusion, unconsciousness and death.
It is important to treat all DCS as serious, even pain only!
First aid and treatment of DCS
Oxygen is recommended for DCS first aid treatment because it may accelerate nitrogen elimination and raise blood oxygen levels, reduce limb pain, and reduce bubble size.
Administer oxygen to the patient, this helps to accelerate the nitrogen elimination from the tissues and raises blood oxygen levels. This assists tissues with blood flow that was reduced by bubble blockage.
Keep breathing patients lying level on the left side with the head supported in the recovery position. This helps to keep the airway clear if the patient vomits and also to ensure blood flow to the brain. Advise the patient not to sit up even during transport or if feeling better.
Lay a non-breathing patient on the back to provide rescue breathing (learnt from EFR), whilst also using the continuous flow with a pocket mask for rescue breaths if possible. Monitor the airway, breathing, circulation and contact emergency medical care.
Recompression chamber treatment is required as this forces the bubbles in the patient’s body to a small size or back into solution. It alleviates symptoms by effectively removing the immediate cause.
Attempting recompression in the water is not advised due to the depths and times required and also the lack of access to necessary drugs. Additionally, putting the patient back into the water to re-compress for less than the required time and depth will just make them worse.
Both DCS and lung over-expansion injuries (discussed later) require the same first aid, there’s no need to distinguish between them when providing care. Decompression Illness/ DCI therefore refers to both DCS and lung over-expansion injuries as a single condition with respect to the emergency protocols and first aid.
Factors Predisposing a Diver to DCS
Individual variations in physiology may affect the risk of decompression sickness. This along with the actions taken by the diver creates predisposing and preventative factors with respect to DCS.
Body fat: Nitrogen in more soluble in fat than water and so a diver with excessive body fat may absorb more nitrogen during a dive than predicted by a decompression model (tables).
Exercise: Intense exercise more than 12 hours before a dive has been found to have a protective effect. However, intense exercise immediately before a dive seems to predispose a diver to DCS as exercise alters and accelerates circulation it appears to affect absorption and elimination of gas.
Age: Due to natural changes with age, circulatory and respiratory systems for example may work less efficiently, thus interfering with gas exchange. Also, older people tend to have higher body fat.
Dehydration: This reduces the quantity of blood available for gas exchange. Slowing gas removal from the body.
Injury and Illness: Any condition that affects normal circulation can potentially affect inert gas elimination by the body. Healed injuries may produce local circulation problems, and illness can produce a general reduction in circulatory efficiency.
Carbon dioxide: Elevated levels from skip-breathing may interfere with gas exchange by dilating capillaries and increasing or altering gas uptake.
Cold: If a diver becomes cold during a dive (that is starts the dive warm and then gets cold), it means that the diver would have normal circulation whilst taking up inert gas, but restricted circulation while eliminating inert gas.
Altitude and flying after diving: Reduced atmospheric pressure at altitude increases the pressure gradient (the pressure difference) between the gases dissolved in the tissues and ambient pressure.
Patent Foramen Ovale (PFO): Basically a hole in the heart between the two chambers.
History of DCS: The first incident of DCS could injure or degrade the body system, and so making a diver more predisposed to it.
The majority of these predisposing factors, somehow result in, or cause a change in circulation.
Lung Over-Expansion Injuries
When a person breathes from scuba, the lungs equalize with each breath. This situation changes, however, if during ascent the person holds their breath or if an abnormal physiological condition traps air (gas) in a section of the lung. In these instances, declining pressure and expanding air will almost always cause lung over expansion injuries (ascending lung barotraumas- more about barotraumas later)
Air Embolism: is the most serious injury that happens if air enters the bloodstream through the ruptured alveoli into the pulmonary capillaries. This can also be referred to as an arterial gas embolism- AGE.
Air entering the bloodstream in the lungs flows through the pulmonary veins to the heart, through the left side of the heart into the aorta and arterial system. The air bubbles can lodge virtually anywhere in the body’s circulatory system and cause severe damage by stopping blood flow to the tissues.
If bubbles find their way into the carotid arteries, they will go to the brain and cause cerebral air embolism. The bubbles deny the brain oxygenated blood which causes a stroke.
Symptoms include unconsciousness, dizziness, confusion, shock, personality change, paralysis and death. The effect of cerebral air embolism tend to be rapid, compared with DCS which tends to be somewhat delayed.
Pneumothorax: if an over pressurized lung tears along its surface, the expanding gas leaks between the lung and the chest wall (known also as the pleural lining), collapsing the lung either partially or entirely. A collapsed lung is called a pneumothorax.
By itself, it is not immediately life threatening as the victim still has use of another lung. The collapsed lung however with cause pain and may cause the victim to cough up frothy blood.
Mediastinal emphysema: Gas accumulates in the mediastinal (centre of the chest). It is far less serious than either air embolism or pneumothorax.
The accumulating air presses on the heart and major blood vessels interfering with circulation.
A victim may feel faint and short of breath due to this impaired circulation..
Subcutaneous Emphysema: occurs frequently with mediastinal emphysema when the air migrates from the mediastinum, following the path of least resistance into the soft tissues at the base of the neck. Here, air accumulates directly under the skin, causes the victim to feel a fullness of the neck and to experience a voice change. The skin may crackle if touched.
Nitrogen Narcosis
Whilst diving, gases dissolve into the blood and reach the nervous system through the circulatory and respiratory systems. Partial pressures of nitrogen and oxygen increase with depth, and typically at 30m or a PN2 of 3.2bar, high concentrations of nitrogen in the nerve cells result in a type of euphoric, anesthetic effect. Susceptibility varies by the diver and physiological state during dive. It is believed that it results from the disruptions in the transmissions between nerve cells.
It is typically subtle at this depth with slowed thinking, increased problem solving times, a mild sense of euphoria or wellbeing. Other possible symptoms may include drowsiness, false sense of security, poor judgment, lack of coordination, hallucination and giddiness.
Narcotic effects will continue to increase with depth. Narcosis itself isn’t harmful, the concern is a diver’s reduced problem solving ability and slower reaction times affect decisions relating to safety. Symptoms will decrease by simply ascending to shallower depths.
Excessive Heat – Heat Exhaustion and Heat Stroke
The normal body temperature is approximately 37 degrees C, and this is vital for the chemical processes to continue to function within the body.
Too much heat is generally not an issue when diving, as even warm water will eventually cool the skin. It is generally before and after a dive that too much heat becomes an issue, when divers wear
heavy exposure suits out of the water as they interfere with the body’s ability to cool itself.
Initially, skin capillaries dilate (become larger, wider or expand). This allows heat from the blood to radiate through your skin and so this is why a person becomes red (especially in the face) when they become hot- the blood is now flowing more closely to the surface of the skin.
Then perspiration begins, cooling the skin and thus your blood through evaporation.
If the core temperature remains high, the heart rate and pulse accelerate to circulate blood more rapidly to your skin for cooling accompanied by a breathing increase.
Strenuous activity in the sun accompanied with wearing a heavy exposure suit can lead to heat exhaustion, when body works at a maximum capacity to keep your core temperature from rising. A diver suffering from heat exhaustion will have weak and rapid breathing, a weak pulse, and cool clammy skin. They will also sweat profusely thus dehydrating, and become nauseous and weak.
If a diver with heat exhaustion remains hot or continues to heat, the physiological control mechanism will eventually fail and result in heat stroke. The victim’s pulse is strong and rapid, perspiration ceases and the skin is flushed and hot. Without treatment can result in brain damage, organ failure and even death.
Whilst waiting for emergency services, the diver’s exposure suit should be removed and any other clothing, shade needs to be provided and aggressive cooling with misting, sponging and fanning.
Hypothermia
As learned from physics, water conducts heat more than 20 times faster than in air, meaning that temperatures that are comfortable in air may be become uncomfortable and cool in water.
As the body cools, temperature centres in your hands, feet and head trigger heat conserving responses that begin with a change in circulation. Blood flow to your extremities (except your head) slows through vasoconstriction (constriction of blood vessels), this reduces heat loss through the skin. Fingers and toes may become numb after long exposure to the cold.
If vasoconstriction does not sufficiently sustain the core temperature, the body reacts by shivering which generates heat through muscle movement and accelerated metabolism.
In the air, shivering can usually protect the core temperature for a period of time, in water however, the body will reach the limits of its ability to maintain the core temperature. This results in hypothermia.
If shivering is ignored and diving continued, as well as continued shivering, the core temperature will drop and possibly lead to hypothermia.
Mild hypothermia starts with uncontrollable shivering and impaired coordination, along with a reduction in core temperature which lowers to 34 degrees C.
As it advances, uncontrollable shivering and vasoconstriction stop. This is because the body’s heat regulation fails. When this happens, the diver will suddenly feel comfortable as warm blood flows to the skin. This is dangerous because as the diver no longer feels cold, the body is losing heat at an uncontrolled heat and the core temperature drops rapidly.
If this continues there is a decline in mental process, and the diver becomes drowsy, uncoordinated and forgetful. The diver loses consciousness, falls into a coma and eventually death.
For a diver with mild hypothermia, remove any wet clothing and wrap in insulating clothing/blanket, and drink a warm, non-alcoholic drink.
Whilst waiting for emergency services to arrive for a diver suffering severe hypothermia, apply the above but also monitor breathing and circulation. CPR and rescue breathing may be necessary.
 The Ears (see pages 5-28 – 5-32 of the Encyclopaedia of Recreation Diving for more detailed diagrams of the ear)
The Ears (see pages 5-28 – 5-32 of the Encyclopaedia of Recreation Diving for more detailed diagrams of the ear)
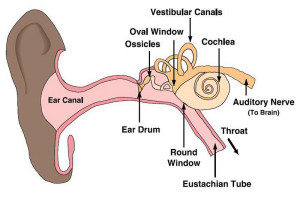
Hearing occurs when sound waves are collected by the ear as vibrations which are passed to the cochlea where they are transmitted as electrical signals which are then decoded by the brain.
The ear has three parts, the external, middle and inner ear.
The outer ear is made up of the pinna (the fleshy part on the side of your head) and the ear hole or ear canal. It is open to air and water pressure. The pinna collects the sound and directs it into the ear canal towards the ear drum membrane.
The ear drum (or tympanic membrane) is the start of the middle ear and is sealed against air and water. The ear drum vibrates when sound hits it. The vibrations from the ear drum are passed onto three small bones (the smallest in the body) called the ossicles. These middle ear bones amplify the sounds and pass them into the inner ear.
The inner ear contains the shell like structure called the cochlea, this is an organ filled in part with a liquid called perilymph. The ossicles attach to the oval window of the cochlea and flexes in and out in response to ossicle vibration. As the oval window flexes, it pushes against the perilymph causing pressure waves to oscillate through the cochlea, in turn stimulating nerve ending in the cochlea which are turned into nerve impulses and sent to the brain by the auditory nerve.
The round window acts as a pressure compensator. It flexes outward when the oval window flexes inwards against the incompressible perilymph, and so flexing inward when the oval window flexes outward. Without this compensating action, vibration could not be transmitted as a pressure wave and hearing could not take place.
The vestibular canals (sometimes known as the semicircular canals) control balance as well as a sense of orientation. They do not contribute to hearing but are connected to the cochlea, and pressure changes result with responses to balance as well as hearing.
Ear responses to pressure concern the middle ear as it is dry and air filled. It connects to the Eustachian tube (connected to the throat) which allows gas to flow from it. The outer ear is open to the environment and so always in equilibrium with the surrounding pressure. The inner ear is entirely fluid filled and therefore unaffected by pressure.
Pressure Changes on Body Air Spaces
Barotrauma is a pressure related injury which results from a squeeze and is cause by the failure to equalize and air space. Any air space can suffer from a barotraumas. Descending barotraumas are called squeezes and ascending barotraumas are called reverse squeezes, reverse blocks or expansion injuries.
Squeeze: involves the hydrostatic pressure forcing body tissues into uncompensated air spaces. So we can say that the pressure on the outside is greater than the pressure on the inside. It is the phenomenon of a shrinking air space as the pressure rises and the volume reduces during descent, causing pain to the diver.
Reverse Block/Squeeze involves trapped expanding gas forcing tissues apart as hydrostatic pressure declines. Some ascending barotraumas involve expanding gas forcing its way into the blood stream
(e.g. lung overexpansion injuries). As the air expands during ascent, it needs to find a release. If this is prevented it can cause serious pain and injury.
Ear Problems:
If a diver descends too far without equalizing, increased air-pressure differential between the middle ear and the gas in the throat may pinch the Eustachian tube shut, making it impossible to equalize. The most common cause of equalization problems is congestion due to a cold or allergy.
Middle ear squeeze: If a diver descends whilst unable to equalize, there is a sharp pain in the ear caused by hydrostatic pressure, forcing the ear drum in towards the unequalized air space. If this continues, the pressure forces fluids and blood from the tissues from the tissues surrounding the middle ear into the ear’s air space.
As this happens, the sharp pain diminishes and the diver’s ear feels “full”.
Eardrum Rupture: If a diver with unequalized ear descends faster than hydrostatic pressure forces liquids from the tissues into the middle ear, the eardrum may burst inwards.
When this occurs, the diver feels sharp pain followed by immediate relief as the break allows water into the middle ear instantly equalizing the pressure. As the water temperature is colder than body temperature, it can cause vertigo and disorientation as it cools the vestibular canals.
Reverse Squeeze/Reverse Block: This results when the middle ear equalizes on descent but expanding gas fails to exit by the Eustachian tube on ascent. This happens most frequently when a diver uses decongestants to dive with a cold or allergy and the decongestants wear off during the dive.
It feels similar to a middle ear squeeze except the pressure forces the ear drum outwards. Due to a diver’s limited air supply, eventually the diver must surface, equalized or not.
Ear Plug Problems: Ear plugs create air spaces in the air canals, between the plug and the ear drum that cannot equalize. If a diver were to wear ear plugs, during descent the eardrum would hurt as pressure forces it outwards into the un-equalized space. If the diver tried to equalize it would make the pain worse as adding air to the middle ear increases the pressure difference.
Round Window Rupture: A round window rupture on the cochlea takes place if a diver delays equalization the attempts a forceful Valsalva maneuver (the Valsalva maneuver is a technique when a diver blows against a pinched nose, using the diaphragm to attempt to exhale against the blocked (pinched) nose).
In an unequalised ear, the eardrum flexes inward in response to hydrostatic pressure. The inward movement transmits and amplifies as it travels through the ossicles into the cochlea via the oval window. The oval window presses inward, exerting pressure on the perilymph, and the compensating round window flexes outward. If the diver at the same time equalizes using a forceful or lengthy Valsalva, the perilymph pressure increase combines with the pressure transmitted from the eardrum and can rupture the round window.
The Frenzel maneuver minimizes the probability of round window rupture, but requires more time to master. As opposed to using the diaphragm to attempt to exhale as with the Valsalva maneuver, the Frenzel uses the throat muscles to compress air against the blocked nose.
Sinus Problems:
A diver who descends with blocked sinuses may or may not feel pain as pressure pushes in on trapped gas pockets within the sinuses. If the diver descends rapidly, sinus pain may occur between the eyes, over the teeth or in the cheek bones. The pain usually subsides as hydrostatic pressure forces blood and fluid from the surrounding tissues into the gas pockets thus restoring the pressure balance.
During ascent, the gas reexpands, pushing the accumulated fluids and blood into the nasal cavity. This often causes the diver to surface with blood in the mask, a definite indication of sinus squeeze.
Lung problems:
Air is delivered to a diver at approximately ambient pressure, and so the lungs equalize to changing depth with every breath. The lung volume remains the same as when you breath at the surface. (Lung overexpansion injuries discussed earlier)
Lung squeezes won’t happen if a diver breathes normally. However, it can happen if a person dives to a depth that compresses the lungs below their residual volume (the lowest volume they reach naturally). Although this would mean a free dive deeper than 30m or you hold our breath and descend with empty lungs. This could compress the lungs below residual volume in only 2-3m of water.
Mask and dry suit problems:
Unequalised equipment air spaces can cause injuries, although not usually as bad as squeezes in your natural air spaces. A mask squeeze occurs on rapid descent when the diver doesn’t equalize mask air space by exhaling through the nose. Dry suit squeeze occur in a rapid descent if you don’t equalize the air spaces. Most commonly occurs when a rapid descent when the dry suit inflator is accidently left disconnected.
Find more information here:
- DM/IDC Skill Circuit Training Video’s
- DM/IDC Dive Physics
- DM/IDC Dive Decompression and RDP Tables
- DM/IDC Dive Equipment
Like & Share

